3 Common Mistakes When Injecting Botulinum Toxin

Ever had a patient with puffy eyes or a heavy brow after botulinum toxin treatment? Worried about eyelid ptosis?
Botulinum toxin-A, commonly known as botox, was first used cosmetically in the mid-1980’s. Since then its usage has exploded.
Out of the almost 10 million treatments performed by members of the American Society for Dermatologic Surgery in 2015, 1.8 million were toxin treatments.
However, due to a lack of standardised training, pharma company-led marketing and unregulated practice, there’s significant variance in botox outcomes.
Here we review the three most common mistakes aesthetics practitioners make when injecting botulinum toxin, and how to avoid them…

Mistake 1: Over-treating the frontalis
The frontalis is the hardest area of the face to treat with toxin. It’s the only elevator muscle in the forehead and accurate treatment is required to achieve natural results.
There are a few points to consider when treating the frontalis:
– The dose will need to be adjusted depending on the size of the forehead and the dynamic lines. For example, in a patient with a long forehead, two rows of injections may be required to cover the area sufficiently. In patients with a small, short forehead, a lower dose is advised, especially for the initial treatment.
– Men usually require a higher dose of botulinum toxin compared to women.
– If the three depressor muscles (orbicularis oculi, corrugator and procerus) aren’t treated at the same time, this may result in heavy looking eyebrows. It can also potentially cause brow ptosis.
– Patients who present with increased skin laxity in the upper eyelid and hooded eyelids should be treated with caution. Injections need to be placed highly (at least 3 cm above the orbital rim). If the frontalis muscle is over-compensating for increased skin laxity and is required to open the eyes, toxin treatments in the frontalis muscle should be avoided.
Additionally, when treating the tail of the corrugator muscle, ensure the injection is placed superficially. The muscle inserts into the skin laterally and superficial placement will avoid inadvertent treatment of the frontalis.
Mistake 2: Believing the myths
Many post-treatment instructions are highly anecdotal and speculative. For example, there’s no evidence that keeping the head elevated for 6 hours post treatment reduces the chance of adverse events. In fact, most of the toxin is inside the synaptic vesicles within 5 to 10 minutes after binding.
There have been no demonstrated alterations of effect from massaging or not massaging the areas injected post-treatment, either.
The only study showing that post-treatment muscle activity by a patient can be beneficial, is by Wei et al. This demonstrated that masseteric muscle atrophy was significantly higher in patients who clenched their chewing muscles for two hours per day after treatment. So recommending chewing gum after masseter toxin would be sound clinical advice – although this evidence is very preliminary.
In summary, the below common pieces of aftercare advice have no evidence:
– “don’t rub the area after treatment”
– “avoid applying make-up after treatment”
– “do not lie flat after treatment”
– “avoid air travel after treatment”
In our aftercare advice, we still recommend not rubbing the treated areas and to avoid applying makeup directly over the injection sites. This is because these make sense to us.
Mistake 3: Ignoring the Mid and Lower Face
Botulinum toxin is fantastic for dynamic lines in the upper third. However, as you gain confidence, don’t be afraid to explore some of the more unusual applications of botox in the mid and lower face.
Note – these are off-label treatments.
We believe the following are the most useful muscles to target in the lower face:
Depressor Angulae Oris

This muscle is partially responsible for causing the corners of the mouth to turn downwards at rest.
Two to three units per side at mid-muscle height, in the subcutaneous plane, will result in effective treatment. Importantly, avoid the depressor labii inferioris, which lies deeper and more medially.
Levator labii superioris alaeque nasi and nasal tip droop

The elevator labii superioris alaeque nasi originates from the frontal process of the maxilla and inserts into the skin of the nasal ala and the superior aspect of the lip. This muscle is responsible for elevating the superior lip and the nasal ala.
It also works alongside the depressor septi nasi muscle to open the nostrils.
Gummy smiles can be effectively treated with botulinum toxin. Two units right at the peak of the nasolabial fold, in the subcutaneous plane, will often be all that’s required. This treatment often requires an adjustment dose.
Please note that recent use of filler to affect the action of this muscle can be equally, if not more effective at treating a gummy smile. This process is called myomodulation, and is outside the scope of this article.
Nasal tip droop:
Musculature around the nose is complex and can be divided into the elevators, depressors, dilators, and constrictors.
The levator labii superioris alaeque nasi belongs to the elevator category. The clue is in the name! In fact, the latin translation is ‘elevator of the upper lip accompanying the nose’. Injecting three units in each LLSAN muscle and five units in the depressor septi nasi muscle will prevent the nasal tip from drooping, especially when the patient is smiling.
Masseter
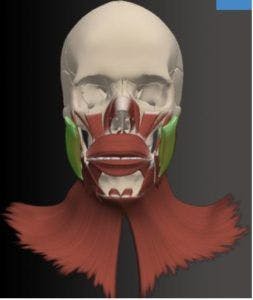
Whilst most of the muscles treated by botulinum toxin relate to facial expression, the masseter is a muscle of mastication. It’s a thick, rectangular muscle with superficial and deep components, originating from the zygomatic arch. The superficial part inserts onto the masseteric tuberosity at the outer surface of the mandibular angle. The deep part runs further dorsally onto the outer part of the mandibular ramus.
This muscle can hypertrophy causing a square-faced appearance. This is usually asymptomatic but can contribute to temporomandubular joint dysfunction and bruxism (teeth-grinding). Toxin will cause atrophy of the muscle, reducing prominence and slimming the jawline.
References:
American Society for Dermatologic Surgery. ASDS survey: nearly 10 million treatments performed in 2015. Available from: https://www. asds.net/_Media.aspx?id=9449. Accessed February 1, 2017.
Botulinum Toxin in Aesthetic Medicine: Myths and Realities
Jeffrey S. Dover, MD, FRCPC,* Gary Monheit, MD,† Mark Greener, BSc(Hons), MRSB,‡ and Andy Pickett, PhDxk
de Sa Earp AP, Marmur ES. The five D’s of botulinum toxin: doses, dilution, diffusion, duration and dogma. J Cosmet Laser Ther 2008;10: 93–102.
Colasante C, Rossetto O, Morbiato L, Pirazzini M, et al. Botulinum neurotoxin type A is internalized and translocated from small synaptic vesicles at the neuromuscular junction. Mol Neurobiol 2013;48:120–7.
Wei J, Xu H, Dong J, Li Q, et al. Prolonging the duration of masseter muscle reduction by adjusting the masticatory movements after the treatment of masseter muscle hypertrophy with botulinum toxin type a injection. Dermatol Surg 2015;41(Suppl 1):S101–9.
Dr Tristan Mehta
Founder and CEO of Harley Academy
Tristan founded Harley Academy to combat the established lack of standardised medical training provided within the speciality. He is a well respected cosmetic physician, CEO of Harley Academy and co-founder of both STORY clinics and Comma, the online global community for medical aesthetics. He created the nationally recognised Ofqual-regulated Level 7 qualification in Injectables.
Dr Yalda Jamali
Clinical Educational Fellow & Mentor
Dr Jamali has previously worked with Harley Academy to develop teaching content and as a lead clinical mentor. Her successful aesthetics clinic in Nottingham reveals her artistic eye for facial aesthetics.
All information correct at the time of publication. Article last fact-checked: 11 January 2023
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners












STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

