The Most High-Risk Injection Zones for Filler, Toxin & Biostimulators

As aesthetic practitioners, it’s vital to be aware of the most high-risk injection zones for the treatments you offer.
We all want to ensure we’re practising to the highest degree of safety with the most up-to-date, evidence-based knowledge. As such, we wanted to bring you some new information on this important topic.
Professor Sebastian Cotofana, esteemed facial anatomist, researcher and Harley Academy’s Academic Director, has recently released key findings on this.
Read on to learn which regions have been identified as the most high-risk injection zones for soft tissue fillers, neuromodulators and biostimulators.

Left, Professor Sebastian Cotofana - Right, Dr Tristan Mehta
“A detailed anatomical knowledge is paramount to safe aesthetic practice”
Professor Cotofana led the Identifying Levels of Competency in Aesthetic Medicine: A Questionnaire-Based Study, published in the Aesthetic Surgery Journal (April 2024).
The international research team included Harley Academy founder and CEO, Dr Tristan Mehta.
Study authors stressed the importance of “detailed anatomical knowledge” as it’s “paramount to safe aesthetic practice.”
The team conducted a community-based online survey, uncovering interesting aspects of aesthetic medicine via social media.
Whilst the primary aim of this study was to “identify levels of competency for the aesthetic practitioner and necessary achievement milestones during the educational path from novice to expert injector”, additional discoveries were made.
Professor Cotofana advises, “A total of 386 respondents from 61 countries provided feedback on various aspects of aesthetic medicine. This included their perception of dangerous and difficult facial regions to treat with soft tissue fillers, toxins and biostimulators.”
Perceived highest-risk filler & biostimulator treatments
The survey responses confirmed that “the aesthetic medical community is in agreement about which facial regions pose the greatest risk for causing severe adverse events when administering soft tissue fillers and biostimulators.”
Facial regions perceived as being the most high-risk for filler treatments and biostimulators were identified as:
1. Nose
2. Glabella
3. Forehead.
“These facial regions have in common that they receive direct arterial blood supply from branches of the ophthalmic artery,” comments Prof. Cotofana. “This opens up the pathway for the injected product to flow backwards into the ophthalmic artery circulation, which includes the various layers of the retina.
“Interestingly, the facial regions that were perceived as most difficult to treat and achieve a perfect aesthetic outcome - if such outcome exists - were, as follows.”
1. Nose
2. Tear trough
3. Forehead.
“This showcases that the tear trough, despite not having a high vascular risk, carries a high degree of difficulty to treat. It’s separating, for the first time, the intrinsic risk - facial danger zones - from procedural risk.”

Most high-risk toxin treatment areas based on perception
For botulinum toxin injections, the treatment zones perceived to be the most risky for causing adverse events were:
1. Perioral
2. Forehead
3. Masseters.
Prof. Cotofana states, “This showcases that these facial regions are most frequently associated with toxin-related adverse events… More research needs to be conducted.”
When asked about the facial regions respondents considered most difficult to treat with neurotoxins to achieve a perfect aesthetic outcome, the results were:
1. Perioral
2. Jawline
3. Forehead.
“Again, the perioral region was listed first,” notes Professor Cotofana. “This emphasizes the need for the aesthetic research community to focus on this region.”
Further research is needed, especially into the lower face
He concludes, “For daily clinical practice, the results of this study provide insight into the injector community's perception of risk and ease for various injectable treatments. Future studies will need to focus more on the lower face to address those needs.”

Why non-surgical rhinoplasty is a high-risk injectable treatment
Non-surgical rhinoplasty is also known as a liquid nose job or nose filler. It can be used to contour the nose and smooth bumps or dorsal humps. Whilst its effects aren’t as long-lasting as surgical rhinoplasty, it can be a useful treatment with beautiful outcomes in the right hands.
Nose filler is an advanced aesthetic treatment due to the high level of vascular, so procedural risk. A high level of skill and expertise is required to achieve natural-looking and aesthetically pleasing outcomes.
It should not be attempted by unqualified, inexperienced cosmetic injectors without specific rhinoplasty training.
Nasal anatomy
One reason non-surgical rhinoplasty is considered an advanced treatment is the complex vascular nature of the nasal anatomy.
The nose is a complex structure with multiple cartilage and bone components that interact to form its shape. This area is rich in blood vessels, heightening the potential for vascular complications.
The nose receives blood from both the internal and external carotid arteries. The arteries include:
- Angular artery: This vessel supplies blood to the medial aspect of the nose and the lower eyelid
- Nasal artery: A branch of the internal maxillary artery, it supplies blood to the lateral and dorsal aspects of the nose
- Septal artery: This artery supplies blood to the nasal septum.
Possible complications from non-surgical rhinoplasty
Injecting fillers into the nasal region requires a concrete understanding of facial anatomy and the potential effects of the filler on these structures. Missteps can lead to undesirable results, such as asymmetry, overcorrection and vascular complications.
The risks of filler complications associated with non-surgical rhinoplasty should not be underestimated. Cosmetic injectors must be aware of the potential for adverse events, including:
- Vascular events: Vascular occlusion can occur when dermal filler blocks blood flow directly or indirectly to the nose, leading to tissue necrosis and scarring - and in very rare cases, blindness
- Infection: The injection site can become infected, especially if proper aseptic non-touch technique is not followed
Temporary or permanent disfigurement: The concerns above, plus if dermal filler is injected incorrectly or in excessive amounts, can cause long-term aesthetic issues.
Why the forehead can be a high-risk area for aesthetic treatments
The most common injectable treatment administered to the forehead is botox. Hyaluronic acid and biostimulatory fillers can be used in this area, as can skin boosters.
Leaving skin boosters aside, let’s focus on the products injected at a deeper level - fillers and toxins.
Whilst forehead botox is fairly common and can be administered by novice aesthetic practitioners, forehead filler is considered a more advanced procedure.
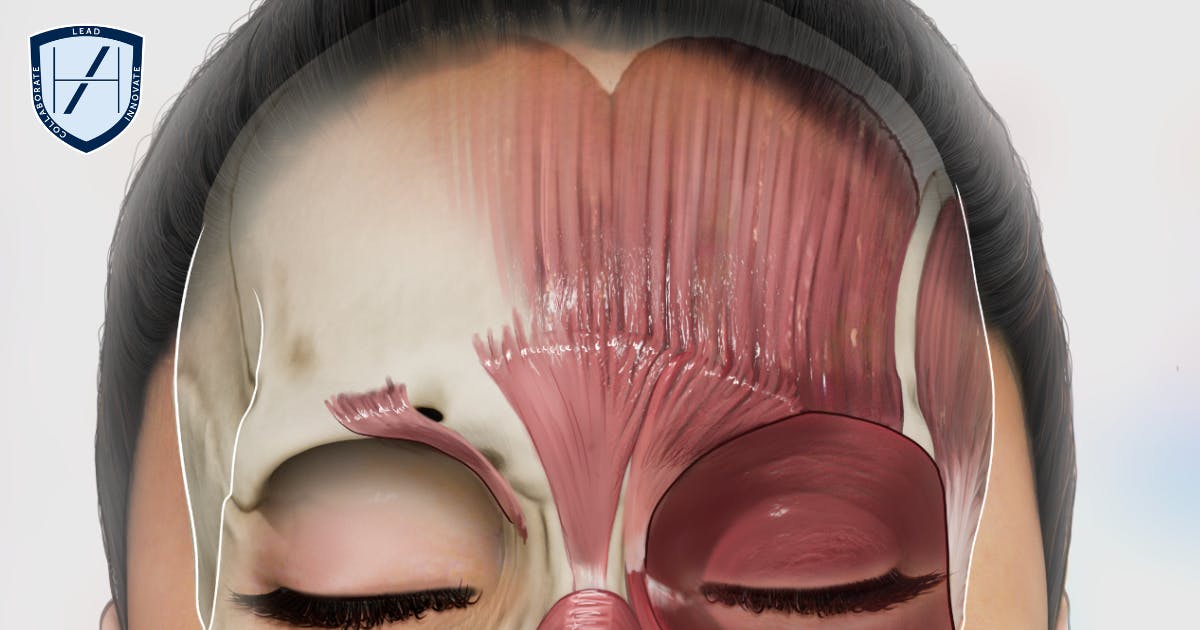
It’s of primary importance to fully understand the anatomy of the region before you start injecting. Not least because the forehead is highly vascular, which makes it a high-risk area for injectables.
Forehead anatomy and potential complications
The forehead is composed of the frontal bone, which is covered by a layer of subcutaneous tissue, muscle and skin.
Underlying forehead musculature plays a crucial role in facial expressions, hence its propensity for rhytids. The frontalis is the primary muscle responsible for raising the eyebrows and creating forehead wrinkles.
This region is traversed by numerous blood vessels, including branches of the supratrochlear, supraorbital and superficial temporal arteries.
The forehead has a rich blood supply, with numerous vessels located relatively superficially. This increases the chance of them being easily damaged during toxin or filler injections.
Veins or arteries:
- Supratrochlear and supraorbital arteries: These arteries supply the upper forehead. The supratrochlear, supraorbital and paracentral arteries could potentially cause ophthalmic complications due to occlusion of the ophthalmic artery
- Frontal branch of the Superficial temporal artery: This prominent artery along the side of the head can be visible in some individuals. Injecting filler into this artery in the central forehead can lead to haematoma. In rare cases it may cause vascular occlusion with potential ophthalmic complications
- Frontal vein: This artery drains blood from the forehead and joins the superficial temporal vein. Injecting into this vein can also cause haematoma or vascular events
Nerves:
The forehead is supplied by supraorbital and supratrochlear nerves. These are branches of the ophthalmic division of the trigeminal nerve which is a sensory nerve.
The frontal branch of the facial nerve supplies motor innervation to the forehead and eyebrow muscles.
Rarely, injecting soft tissue filler can inadvertently damage nerves.
Possible complications from forehead filler
Given the vascularity of the forehead, the risk of complications associated with dermal filler injections is relatively high. These can include:
- Vascular complications: If a blood vessel is punctured or compressed by the filler it can lead to tissue necrosis and potential disfigurement if not addressed. This can also happen if a blood vessel becomes spasmodic. There’s also a risk of ophthalmic complications.
- Asymmetry: Improper filler injection techniques or uneven distribution of filler can lead to asymmetry or distortion of the forehead.

Potential complications from forehead botox
Injecting neurotoxin into this muscle can cause temporary paralysis, leading to a smoother appearance. However, if the injections are not performed correctly or if the dosage is excessive, the muscle may become over-relaxed, resulting in an unnatural or "frozen" appearance.
The main aesthetic risk we are concerned about is brow ptosis from over-treating the frontalis or treating the frontalis in an unsuitable patient.
Getting the balance right to achieve the best ‘wrinkle-relaxing’ results for your patient, whilst avoiding overcorrection is an art. This is taught from your very first aesthetics training courses at Harley Academy. They include:
- Foundation Training in Botox & Dermal Fillers
- The Aesthetics Accelerator
- Level 7 Diploma in Botox & Dermal Fillers.
These courses lay the foundation for your career as a safe and mindful medical aesthetics practitioner.
As with any cosmetic injectables, complications are always a possibility. Whilst having a solid educational foundation in facial anatomy, correct technique and practical mentored injecting practice will help you to avoid them, this only minimises the risk.
Those associated with forehead botox include:
- Eyelid or eyebrow ptosis: Lid or brow drooping can occur following botox injections if the toxin spreads too far outside of its intended target. You can find out more about this in our article on How to Tell Lid Ptosis from Brow Ptosis.
Understanding facial anatomy is crucial for safe aesthetic practice
As Dr Tristan Mehta detailed in our article An Injector’s Guide to Differences in Male & Female Facial Anatomy, this knowledge is crucial for safe aesthetic practice.
Having a solid, working knowledge of facial anatomy is essential for all aesthetic practitioners. This doesn’t only mean studying male and female anatomical structures so you can name and locate key arteries, for example.
You need to have a deep understanding of possible variations in anatomy and when these are likely to occur. As aesthetic medicine is still such a novel medical specialty, research is ongoing which means new findings are coming up all the time.
This is especially true as we as an industry are leaning more towards the use of ultrasound imaging devices. These tools can be immensely useful in determining each patient’s unique facial anatomy including any variances. However, you need to be able to understand how to read ultrasound images to properly incorporate them into your practice. Furthermore, they are certainly not a replacement for current and steadfast anatomical knowledge.
Committing to continual learning and development is vital if you want to have a safe and successful career in medical aesthetics.
You can now join the waiting list for our Ultrasound in Facial Aesthetics course, which we’ll be launching soon.
All information correct at the time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners












STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

