Preventing Filler Embolus And Vascular Occlusion

Our Head of Clinical Governance, Dr Joanna Hackney explains how to prevent filler embolus and vascular occlusion.
Complications and risks associated with soft tissue fillers remain one of the biggest concerns for aesthetics practitioners starting out. And rightfully so! A healthy respect for dermal filler emboli and resulting vascular occlusions will help you keep patient safety at the forefront of your practice.
As medical professionals, most of us will have managed far more sinister, fear-inducing or complex situations. Yet during our toxin and filler Foundation Training courses, I still hear some students muttering, “Well this has totally put me off doing filler” after seeing a photograph of skin necrosis.
Through our Level 7 Diploma in Injectables course, Harley Academy aims to achieve a cohort of students who are well equipped to avoid, recognise and manage such complications.
Here are some of my top tips for preventing filler embolus and vascular occlusion…
Mechanism for Central Retinal Artery occlusion leading to blindness with dermal filler injection
1. Know your facial anatomy
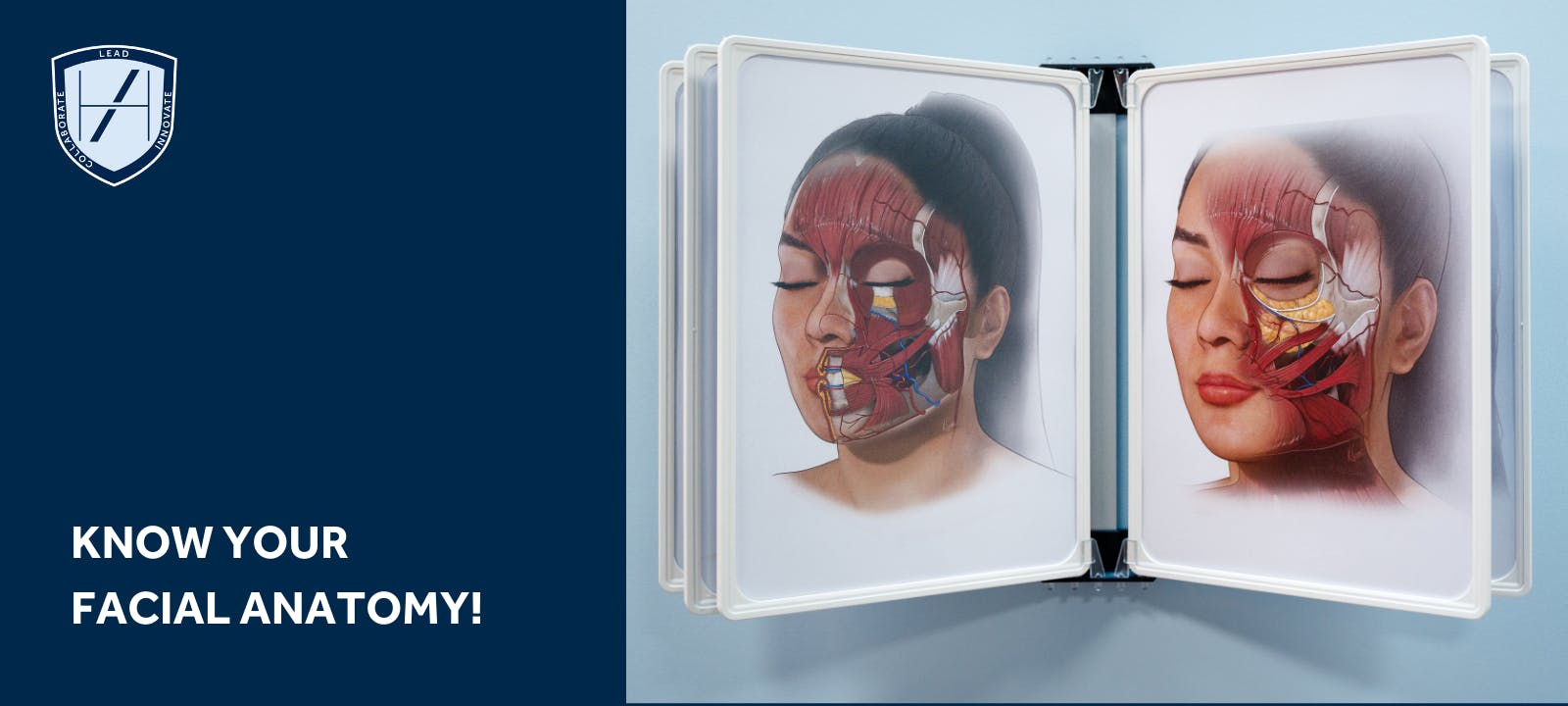
Learn your vasculature, and utilise the ‘layer based’ approach taught at Harley Academy to ensure you are always injecting your filler in the safest plane, at the safest depth and using the safest technique.
In depth knowledge of named facial vessels and their branches is mandatory for injectors, particularly when treating more ‘high risk’ areas, such as the nasolabial fold, where increased caution and attention to depth and technique is key.
2. Aspirate
This may be a more controversial suggestion due to the risk of reassuring ‘false negatives’. Most practitioners, however, will have anecdotal or personal experience of a positive aspirate, so the merit of aspiration should not be ignored.
Low sensitivity should be taken into consideration to avoid practitioners becoming falsely assured by a negative aspirate, and this technique should be used in combination with others to maximise safety.
3. Inject small volumes
Literature suggests minimising bolus volumes. We advise limiting supraperiosteal boluses to a maximum of 0.1ml per area. When injecting off bone, techniques utilising constant movement of the needle tip such as retrograde linear threads and fanning, alongside limiting injection volumes can further reduce the risk of a significant filler embolus.
4. Inject slowly
When injecting boluses supraperiosteally, use a slow injection speed with a low extrusion pressure on the plunger of the syringe. This will reduce the risk of depositing large volumes of filler intravascularly, or causing retrograde filler movement through the vessel against arterial or venous pressure.

5. Consider cannula use
The use of a large bore (25G or lower) blunt tipped cannula can decrease (but not eliminate) the risk of penetrating a vessel wall. Continuous movement and a gentle, non-forceful technique will be of further use with this tool.
6. Beware previous scarring or surgery
Areas of scarring from trauma, previous surgery, or multiple previous treatments can increase the risk of cannulating a vessel. Vessel fixation from scar tissue can prevent arteries from ‘moving out of the way’ when advancing through soft tissue – even when utilising a cannula technique. Beware of injecting in such areas and take a thorough history to establish risk.
You may find our articles on administering filler when a scar is present useful reading.
7. Product choice
Hyaluronic Acid based, temporary dermal fillers do have the advantage of hydrolysing with Hyaluronidase in the event of an occlusion or embolus. This should be reassuring to practitioners, but not provide a ‘safety blanket’ leading to promotion of careless, unsafe techniques.
Viscous, non-reversible products have the additional risk of increasing pressure around the vessels in the area injected, potentially leading to occlusion of the lumen secondary to compressive pressure in that compartment.
8. Progress appropriately!
Practice within your limits. Do not progress to high risk areas until you are suitably experienced.
Of course, statistics may imply that if you perform enough filler cases, you have a good chance of experiencing a vascular event during your aesthetics career. It can happen to anyone.
However, following the steps above will ensure you are treating responsibly, safely and cautiously. Plus you'll also be reducing your margin of risk.
Remember, this rare complication of filler treatment is manageable most of the time. So, due diligence in preventing it is as important as being prepared to recognise and manage it.
For aesthetic practitioners wanting to really boost their confidence in this area, Harley Academy offers a short eLearning course in Preventing and Managing Dermal Filler Complications.
This popular online training course is case-study led. It can be completed in your own time, at your own pace. Because it's online, you can complete it from wherever you happen to be, too - no need to travel to our aesthetics training clinics in London for this one!
Whilst it's also available to purchase as a standalone aesthetics course, we also provide access to this to all our Level 7 trainees, free of charge.
Dr Joanna Hackney
Dr Joanna Hackney is an experienced aesthetic practitioner and clinical mentor at Harley Academy. Before switching to advanced aesthetic medicine, Dr Hackney was an anaesthetist and fellow of the Royal College of Anaesthetists. She is known for the precision of her work, providing balanced and natural-looking results. Her approach prizes patient safety and each individual’s best interests.
All information correct at the time of publication - last updated: 26 April 2024
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners














STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

