New GMC Rules For Aesthetic Medicine And Cosmetic Interventions

The General Medical Council (GMC) and Royal College of Surgeons (RCS) have published new rules for doctors who offer cosmetic interventions. The new rules are emblematic of the shifting tides of regulation in Aesthetics.
The rules focus on patient safety and ethical marketing, and apply to doctors who deliver non-surgical interventions such as botulinum toxins and dermal fillers, as well as surgical cosmetic procedures.
Health Minister Ben Gummer said of the rules:
“This new guidance for doctors is an important step forward in improving standards and ending the lottery of poor practice in parts of the cosmetic industry.”
Harley Academy welcomes the new rules. Indeed, they are are the same best practices that we have always been teaching on our Botox and Dermal Filler courses.
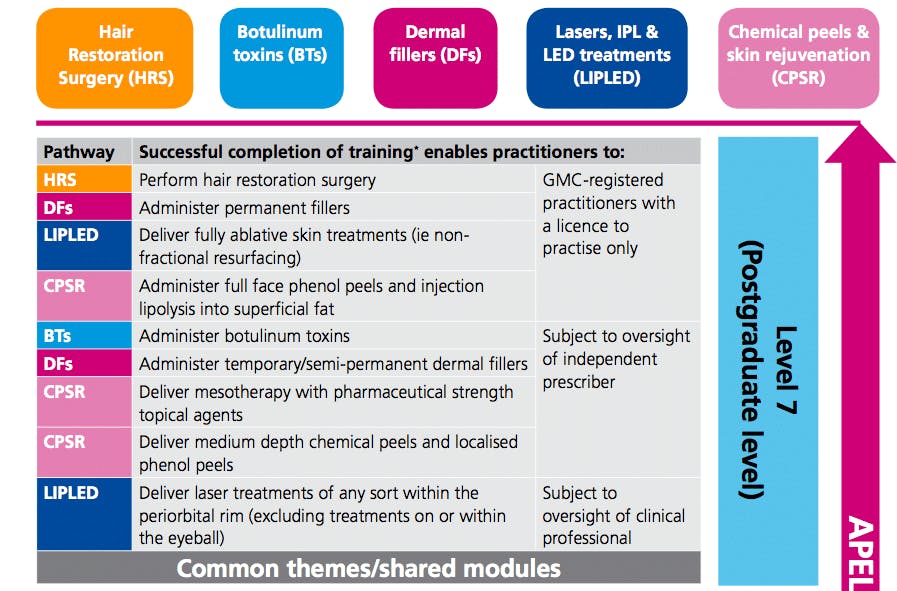
Fortunately for our students, the new GMC rules explicitly cite the HEE Guidelines for the level of education Aesthetics practitioners should attain before 2018.
Harley Academy courses are built around HEE’s Qualification Requirements for the Delivery of Cosmetic Procedures, which, like the new GMC rules, incorporate recommendations from the Keogh Review of the regulation of cosmetic interventions.
What are the new rules?
1. Witness patient consent yourself
It is essential to a shared understanding of expectations and limitations that consent to a cosmetic intervention is sought by the doctor who will perform it, or supervise its performance by another practitioner.
2. Give patients an appropriate amount of time for reflection
Make sure patients are given enough time and information before they decide whether to have an intervention
How do you calculate an appropriate amount of time? The GMC say the time will vary depending on the invasiveness, complexity, permanence and risks of the intervention. For injectable treatments, these will be at the lower end of the scale.
3. Consider your patient’s psychological needs
You must satisfy yourself that the patient’s request for the cosmetic intervention is voluntary.
4. Work within your competency
Before carrying out an intervention for the first time yourself, or supervising others performing it, you must make sure you can do so safely, eg by undergoing training or seeking opportunities for supervised practice.
Seek advice or refer on when necessary.
5. Inform patients of the risks
Make sure patients have the information they want or need, including written information that supports continuity of care and includes relevant information about the medicines or devices used — and this should be done at the outset, not after the treatment.
What else counts as a risk? The failure of an intervention to achieve the desired aim.
6. Take care with children and young people
Make sure younger patients want the procedure themselves, irrespective of whether their parent(s) consent to it.
7. Market honestly and responsibly
You should be able to attract patients without making unjustifiable claims about interventions, trivialising the risks involved, or using promotional tactics that might encourage people to make ill-considered decisions.
What next?
The rules come into force on 1st June 2016. Until other regulatory bodies such as the Nursing and Midwifery Council (NMC) publish their own rules, we recommend that nurses, midwives dentists and other professionals working in aesthetics follow the GMC guidance.
You can find out more about how to consult and treat cosmetic patients in-line with the new GMC rules and HEE guidelines on a Foundation Training course, and in our comprehensive postgraduate level online syllabus.
Further reading:
BBC coverage Clampdown on cosmetic surgery cowboys
Guardian coverage Cosmetic treatment industry given strict rules to protect vulnerable
RCS Professional Standards (PDF)
GMC rules (PDF)
Summary of HEE Guidelines
All information correct at the time of publication