How to Manage Dry Eye Botox Side Effects

Potential dry eye Botox side effects were first added to the medication’s label in October 2024.
Here we explain what you, as an aesthetics practitioner, can do to help to prevent, identify and manage dry eye side effects from Botox injections.
New dry eye Botox side effect information
The FDA circulated the following October 2024 approved updates to the Botox Cosmetic product label. These relate to the use of the Allergan Aesthetics neurotoxin for aesthetic purposes.
“There have been reports of dry eye associated with BOTOX Cosmetic injection in or near the orbicularis oculi muscle. If symptoms of dry eye (e.g., eye irritation, photophobia, or visual changes) persist, consider referring patients to an ophthalmologist [see Warnings and Precautions (5.9)].”
You can read the full label information, including the recommended Warnings and Precautions section on the FDA’s dedicated webpage.
What is ‘dry eye’?
Dry eye is a multifactorial condition also known as dry eye syndrome (DES), dry eye disease (DED), ocular surface disease (OSD), dysfunctional tear syndrome (DTS) or keratoconjunctivitis sicca.
It occurs when your eyes don't produce enough tears (aqueous deficient), the tears evaporate too quickly (evaporative) or both. There is a loss of homeostasis of the tear film, leading to a lack of adequate lubrication and inflammation of the ocular surface. This can cause a variety of uncomfortable symptoms as well as visual disturbance.
Symptoms of dry eye syndrome
- Burning or stinging sensation
- Scratchy or gritty feeling
- Blurred vision
- Sensitivity to light
- Eye fatigue
- Redness
- Mucus in or around the eyes.
Causes of Dry Eye
There are several factors - not including Botox treatments, which we’ll come on to - that can contribute to dry eye. These include:
- Age: Tear production naturally decreases as we age
- Sex: Dry eye is more common in women due to the hormonal effects on the lacrimal and meibomian glands
- Environmental factors: Dry air, wind, and pollution can accelerate tear evaporation
- Medications: Certain medications, such as antidepressants and antihistamines, can reduce tear production
- Medical conditions: Autoimmune systemic conditions including Sjogren's syndrome and lupus can affect the tear glands. Skin and general medical conditions such as eczema and diabetes can also contribute
- Ocular allergies
- Lifestyle factors: Prolonged computer use, long term contact lens use, smoking and inadequate blinking can contribute to dry eye.

Which Botox treatment areas are linked to dry eye?
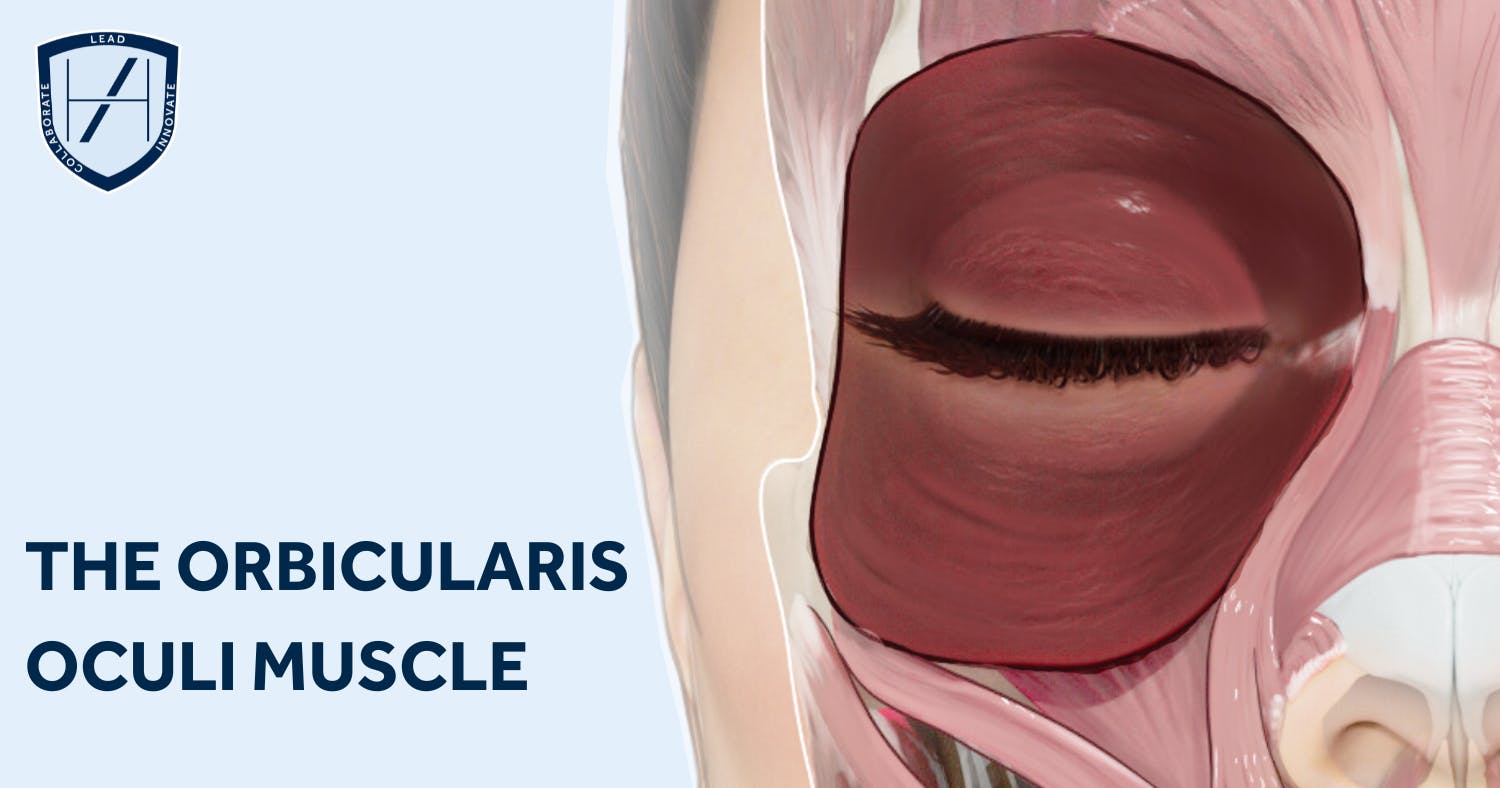
As the update states, it concerns treatments that involve injecting “in or near the orbicularis oculi muscle”.
The orbicularis oculi muscle is a complex muscle surrounding the eye orbit. It’s located superficially, directly beneath the skin surrounding the eye. This means you’d be treating the lateral canthal lines, more commonly known as crow’s feet.
About the orbicularis oculi muscle
The orbicularis oculi plays a crucial role in facial expression, eyelid protection and tear drainage.
Dysfunction of this muscle can lead to various conditions including lid ptosis, incomplete eyelid closure and tear drainage difficulties. The latter can contribute to dry eye syndrome.
The orbicularis oculi muscle is innervated by the temporal and zygomatic branches of the facial nerve (CN VII). It overlies other facial muscles such as the corrugator supercilii and blends inferiorly with the malaris muscle, when present.
The orbicularis oculi muscle consists of three parts:
- Orbital
- Palpebral
- Lacrimal.
The orbital part originates from the medial orbital margin, medial palpebral ligament and lacrimal bone. This is responsible for forceful closure of our eyelids.
The palpebral part originates from the medial palpebral ligament and lacrimal bone. This is responsible for gentle eyelid closure.
The lacrimal part originates from the posterior lacrimal crest and anterior lacrimal bone. This assists in tear drainage by compressing the lacrimal sac.
Links between orbicularis oculi dysfunction and dry eye
Dysfunction of the orbicularis oculi muscle can cause or contribute to dry eye syndrome in a number of ways.
1. Impaired tear film distribution:
- Incomplete lid closure: Weakness or paralysis of the orbicularis oculi can lead to incomplete eyelid closure, known as lagophthalmos. This prevents proper spreading of tears across the ocular surface, resulting in dry spots and discomfort
- Reduced Blinking: The muscle's role in blinking helps to distribute tears evenly and remove debris from the eye's surface. Reduced blinking frequency, often associated with muscle weakness, can lead to tear film instability and dry eye symptoms.
2. Disrupted tear drainage:
- Lacrimal pump dysfunction: The orbicularis oculi muscle contributes to the "lacrimal pump" mechanism, which helps drain tears into the tear ducts. Weakness of this muscle can impair drainage, leading to excessive tears (epiphora) or pooling of tears on the eyelid margin, which can exacerbate dry eye symptoms.
3. Exposure keratopathy:
- Corneal damage: In severe cases of orbicularis oculi dysfunction, the cornea may be exposed to the environment for prolonged periods. This can lead to corneal damage, inflammation, and further worsening of dry eye symptoms.
Conditions affecting the orbicularis oculi and dry eye:
- Facial nerve palsy: Damage to the facial nerve, which innervates the orbicularis oculi, can cause weakness or paralysis of the muscle, leading to dry eye symptoms
- Ageing: As we age, the orbicularis oculi muscle can weaken, contributing to age-related dry eye
- Blepharoplasty: Surgical removal of a portion of the orbicularis oculi muscle during eyelid surgery can sometimes lead to dry eye as a side effect.

Can you prevent dry eye Botox side effects?
Prevention of dry eye Botox side effects comes down to understanding the patient context, the function of the orbicularis oculi muscle and adapting treatment plans accordingly. If there is baseline dry eye, it may be inappropriate to treat with Botox in this muscle as this will make symptoms and potential sequelae worse.
One thing you can do is to consider the risk factors for dry eye - which we’ve listed above - during your patient consultation. Discuss this with your patient prior to them consenting to treatment. You may choose to not treat or treat with a lesser dosage to reduce the impact of treatment.
Additionally, we would always promote the use of best practice toxin injection techniques to help increase the safety of your treatments. We’ve provided information on this below so you can refresh your knowledge.
How to manage dry eye Botox side effects
Dry eye treatment depends on the severity of the condition. Common approaches to managing this condition include:
- Artificial tears: Use eye drops to help lubricate the eyes and relieve symptoms
- Lid hygiene: Advise your patient to clean their eyelids regularly to help remove debris and bacteria that can contribute to dry eye and delay recovery
- Lifestyle changes: Taking breaks from digital screens, using a humidifier and avoiding dry environments can help to alleviate symptoms and prevent further discomfort.
Early intervention can assist in preventing complications. This includes early referral to an Ophthalmology service especially with moderate to severe, or persistent symptoms.
Best practice crow’s feet Botox injection techniques
Clinical trainer and aesthetic nurse practitioner, Kate Smith, has previously detailed How to Treat Crow’s Feet.
“The orbicularis oculi muscle plays a crucial role in the formation of crow’s feet lines,” she notes. “This circular sphincter muscle surrounds the eye and acts as a depressor when activated.
“The main function of the orbicularis oculi muscle is to close the eyelids, which occurs when the muscle contracts.
“Contraction of the muscle also assists in draining tears from the eyes via the lacrimal gland pump system. This is important when considering patients with oedema around the eye area.” With these patients, consider not treating or reducing the toxin dose so as not to worsen any present oedema.
She also provides the following advice on crow’s feet Botox injection techniques.
- Inject superficially into the dermis approximately 1 cm away from the orbital rim
- The licensed Botox dose for lateral canthal lines is 4 units per point, at 3 points, with a total of 12 units per side
- Take care to ensure injections are not placed too close to the orbital rim, so that the ocular muscles are not affected and the eye can perform it’s aperture function
- Ensure you don’t inject too deep at the lower aspect, so that the smile muscles are not affected
- Don’t inject too deep at the upper aspect, so that the lacrimal gland is not affected.
She also recommends considering other options for managing crow’s feet alongside botox plans. These can include topical skincare - particularly daily SPF - and cosmetic dermatology treatments such as microneedling.

Botox courses for medical professionals
As this update proves, there is no substitute for solid medical knowledge, including a detailed understanding of facial anatomy, in aesthetic practitioners.
If you’re a doctor, dentist, nurse or clinical pharmacist looking to get started in aesthetics, we offer a range of botox courses tailored to you.
Build on your existing medical knowledge and skills with specific information relating to facial anatomy, face and skin ageing, cosmetic treatment modalities, patient assessments, product choice and dosing plus safe administration techniques and aftercare.
If you’re looking for a botox course near you, check out our range of aesthetics courses, each of which includes at-home eLearning and in-clinic practical training. From our foundation-level springboard courses to our full, Ofqual-regulated, JCCP-approved postgraduate qualification, the Level 7 in Cosmetic Injectables, you’ll find an option to suit.
If you’d rather talk to someone to get personalised advice on the best aesthetic medicine training course for you, just book a call with our Course Advisors.
We hope this update was helpful and, if you’d like more information on botox injection techniques, check out the rest of our Aesthetic Medicine Articles!
All information correct at time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners














STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

