Managing Herpes Reactivation in Aesthetics Patients

Herpes reactivation is a rare hyaluronic acid (HA) complication from aesthetic medicine treatments. Despite being rare, practitioners must be confident in their knowledge to prevent, diagnose and manage in-clinic cases successfully.
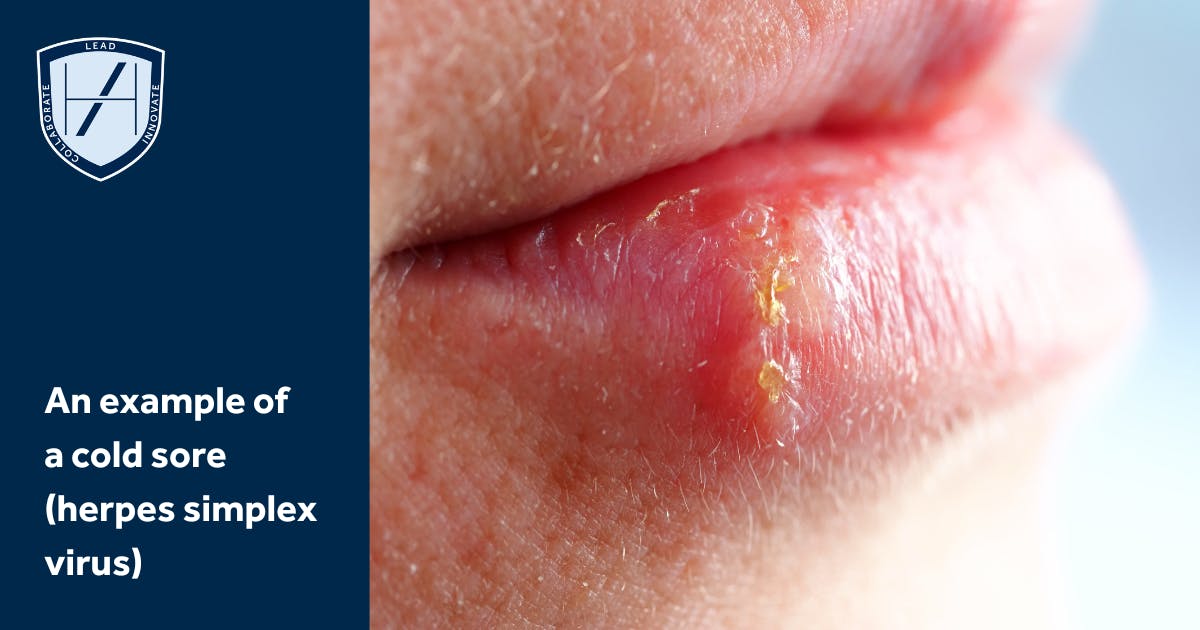
The herpes simplex virus (HSV) is a common infection and affects 67% of people under 50 globally, according to the World Health Organization.
Two types of HSV (HSV-1 and HSV-2) exist. The type that applies mostly to medical aesthetics patients, which causes the common cold sore, is HSV-1. Infection is usually self-limiting. Following infection, the virus lies dormant in the dorsal root ganglion.
Reactivation can be caused by physical trauma, including needle trauma and some more invasive skin procedures.
Read on to discover what injectors need to know about HSV-1 reactivation, how to prevent it and treatment options.

Why does herpes reactivation occur in aesthetic patients?
As with any injectable treatment, the risk of complications is ever-present. With regards to HSV, numerous possible reasons have been suggested as to why herpes activation may occur in aesthetic patients. These include:
1. Damage or trauma from the needle to the nerve fibre
2. Tissue manipulation while injecting
3. Dermal injury
4. Inflammatory reaction after injection
5. Immunosuppression
6. Systemic stress.
How is herpes reactivation present in medical aesthetics patients?
Signs of activation will occur 24-48 hours after injection. It’s crucial aesthetics practitioners advise patients to observe the treatment area closely during this time.
Typically, signs of onset will appear around the injection site in the perioral, lip and nasolabial folds areas. On some occasions, the virus can spread into other areas.
Here are some potential symptoms of an HSV activation that patients should watch out for:
- Swelling
- Redness
- Pain in the injection site
- Itching or tingling
- Crusting.

Can we prevent an HSV activation?
Practitioners should ensure they review a patient’s full medical history in the consultation phase of the treatment process. Here, you should be asking your aesthetics patients questions such as:
- If they've had cold sores before, where, how often and with what triggers
- If they’ve had any past filler injections and if any herpes reactivation arose afterwards
- Whether they are on immunosuppressant medication
- If they have a history of recent cold sores. Have they had any symptoms such as pain, tingling, itching or signs, like vesicles or erythema in the last few days?
If the patient has had a recent herpes infection, it is important to examine the affected region. Treatment should be delayed until symptoms have fully resolved and the skin has fully healed.
If you choose to inject, advise them on what signs to look out for herpes reactivation. This information can be relayed as part of your aftercare advice. Furthermore, always guide your patient to appropriately contact your practice if they begin to notice any changes or pain.
What to do if your patient has a history of HSV
If, during the consultation, you identify that your patient has a history of HSV, oral prophylaxis can be recommended. This should be done after a risk assessment, and if they have no contraindications. In the UK, an example regime is aciclovir 400mg twice a day for seven days, ideally being commenced two days preceding treatment.
Have you considered the differential diagnoses?
It’s important to consider alternative diagnoses such as impetigo and vascular event. These are important differential diagnoses when considering the clinical picture of potential herpes reactivation. For example, in the case of a vascular event, you may also see delayed capillary refill.
What are the best HSV treatment options?
Antiviral options for treating HSV in the UK include oral aciclovir and valacyclovir. Preferably, these need to be started early to be effective. There may also be a need to treat superadded infections, such as impetigo.
Learn to identify, manage & prevent aesthetic medicine complications
As an injector, you must be able to approach patients with confidence and knowledge. Not only does this build your self-esteem as a practitioner but it instils your patient with confidence in you.
At Harley Academy, we understand the multifacetedness of the medical aesthetics industry. This is why we’ve designed a series of courses that are tailored to your specific needs.
Be the gold standard in aesthetic medicine
Our Level 7 Diploma in Botox & Dermal Fillers is an Ofqual-regulated and JCCP-approved, postgraduate level qualification. It allows you to get hands-on experience injecting aesthetics patients in a working clinic, without sharing. You’ll learn all about how to carry out a consultation, administer botox and fillers, plus what aftercare advice to deliver in situ. All of this is done under the guidance of an experienced trainer.
Your practical skills will grow from a solid theoretical base, including essential anatomical and scientific knowledge. This is delivered via our self-paced, interactive and engaging eLearning.
Looking for a focused learning experience and want to boost your confidence in managing complications? Our Preventing and Managing Complications eLearning course will provide you with real-life case studies to learn from. Discover personalised learning paths that align with your medical aesthetics career goals. Book a call with our knowledgeable Course Advisors today.
All information correct at the time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners














STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

