How to Identify and Treat Rosacea as an Aesthetic Practitioner

April is Rosacea Awareness Month; as such we’re discussing how to identify and treat rosacea in your aesthetic practice.
We spoke to clinical trainer, cosmetic doctor, clinic-owner and skin expert, Dr Carol Mastropierro for her insights.
Here we explore rosacea from a medical aesthetics practitioner’s point of view, including the best treatments for rosacea and which skin conditions it can be confused with. Dr Carol also shares when you should refer your rosacea patients to a dermatologist.
Scroll to the end to find a case study where we invite you to test your knowledge by putting together a treatment plan for a patient with rosacea and other aesthetic concerns...

What is rosacea and how does it present?
“Rosacea is a chronic inflammatory skin condition that primarily affects the face,” says Dr Carol.
It has four distinct subtypes, which we’ve outlined below, the most common of which is erythematotelangiectatic rosacea. When we discuss simply ‘rosacea’, this is the condition we’re referring to.
"Rosacea leads to persistent redness, visible blood vessels – telangiectasia - and, in some cases, can affect the eyes and nose. It commonly appears as transient or persistent flushing on the cheeks, nose and/or forehead, together with skin sensitivity with several types of skincare.”
She notes, “Rosacea is a chronic condition, known for its relapsing and remitting nature, meaning symptoms can flare up and then subside before returning again. Flare-ups can be triggered by environmental factors, dietary choices, stress, or changes in skincare routines. While some people may go weeks or months without symptoms, others may experience frequent flare-ups.”
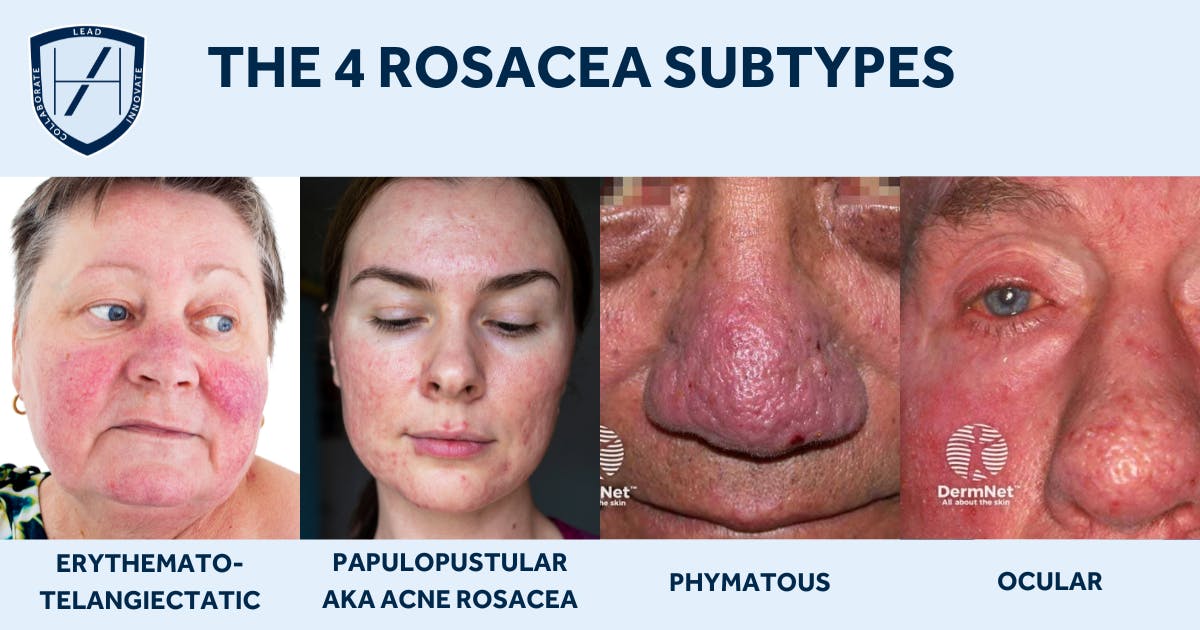
The 4 rosacea subtypes
- Erythematotelangiectatic rosacea: This is the most common form and what people usually refer to when they use the term ‘rosacea’
- Papulopustular rosacea: Also known as ‘acne rosacea’ due to the presentation of papules and pustules
- Phymatous rosacea: A rare phenotype which can lead to thickening of the skin, especially on the nose, causing it to become bulbous. This is known as rhinophyma. May also affect other areas, including the chin, ears or eyelids
- Ocular rosacea: Affecting the eyes with additional symptoms to the expected redness, including irritation, burning, itching, styes or blurred vision.
Mostly affects adult women
Given rosacea is understood to affect around 1 in 10 of all UK adults – with most experiencing mild symptoms – this is a serious consideration for your aesthetic practice.
Research into the epidemiology of rosacea in the UK was published in the British Journal of Dermatology in 2023. It found:
- Rosacea was mostly diagnosed in women (61.5% of the 60,042 cases identified in the study)
- 80% of rosacea diagnoses occurred after the age of 30
- Ocular symptoms were recorded in 20.8% of cases
- Alcohol consumption increased rosacea risks marginally
- Being a current smoker significantly decreased relative rosacea risks.
It's a common misconception that rosacea only affects caucasian skin. Dr Carol busts this myth in our section on genetics, below. Though it's thought that less than 10% of all rosacea cases occur in Black skin, this is likely to be a case of under-reporting.
Common rosacea triggers
“Rosacea is highly reactive to various triggers, which can vary from person to person,” Dr Carol highlights.
She lists some of the most common rosacea triggers as:
- Sun exposure
- Hot or cold weather
- Spicy foods
- Alcohol
- Caffeine
- Cheese
- Stress
- Cardiovascular exercise
- Hot beverages.
“Harsh skincare products containing alcohol, fragrance, or exfoliating acids can also exacerbate symptoms. “
She counsels, “Identifying and avoiding personal triggers is essential for managing rosacea effectively. Keeping a diary of flare-ups can help patients to pinpoint which factors worsen their symptoms and make necessary lifestyle adjustments.”
Is rosacea a genetic condition?
“While rosacea is more prevalent in fair-skinned individuals, particularly those of Northern European descent, it can affect people of all ethnic backgrounds,” shares Dr Carol.
“Although the exact cause of rosacea remains unknown, research suggests that genetics play a significant role in its development. Many people with rosacea have a family history of the condition, indicating a hereditary component.
“However, genetic predisposition alone does not cause rosacea—environmental factors, immune system dysfunction, and the presence of a mite on the skin, known as Demodex folliculorum, can all contribute to its onset and severity.”
The Black Skin Directory has excellent information, with visual examples, detailing how to diagnose rosacea in Black skin.
How is rosacea diagnosed?
“In the UK, rosacea is typically diagnosed by your patient’s GP,” shares Dr Carol. “This involves a facial assessment and an examination of family history and lifestyle factors.
“As a responsible medical aesthetics practitioner with relevant cosmetic dermatology training, you should also be able to diagnose this condition in this way.
“However, for more complex cases and where a biopsy is required, these cases require a dermatology referral.”
Skin conditions that can be confused with rosacea
“Rosacea is often mistaken for other dermatological conditions due to its overlapping symptoms,” confirms Dr Carol. “The most common condition it’s confused with is acne. This can result in misdiagnosis and mistreatment, resulting in a worsening of the patient’s rosacea symptoms.”
“Unlike acne, rosacea does not produce comedones - blackheads or whiteheads - and is more associated with persistent redness rather than oiliness and breakouts.
“Seborrheic dermatitis, another common lookalike, tends to cause flaky, greasy skin, particularly around the nose and eyebrows, whereas rosacea presents more with flushing and sensitivity.
“Lupus, an autoimmune condition, can cause a butterfly-shaped rash on the face, but it’s usually accompanied by systemic symptoms such as joint pain and fatigue.
She stresses, “A correct diagnosis is crucial for effective treatment, and patients should consult a specialist to ensure they receive appropriate care.”
Are rosacea and acne linked?
“Although rosacea and acne can sometimes appear similarly, they are distinct conditions with different causes,” explains Dr Carol.
“Rosacea is primarily an inflammatory and vascular disorder, whereas acne is associated with excess oil production, clogged pores, and bacterial overgrowth.
“However, some forms of rosacea, such as papulopustular rosacea, present with pus-filled bumps that resemble acne breakouts.
“Unlike traditional acne, these blemishes are not caused by blocked sebaceous glands and do not respond to typical acne treatments such as benzoyl peroxide. In fact, some acne treatments can worsen rosacea, making it essential to differentiate between the two conditions for proper management.”
Can rosacea affect the eyes?
Did you know that rosacea can affect the eyes? Not only that, but when it does, you’ll need to refer your patient onwards for appropriate care.
Dr Carol advises, “It can affect the eyes in a condition known as ocular rosacea. This manifests as redness, irritation, dryness, a burning sensation, and a feeling of grittiness in the eyes. In more severe cases it can lead to swollen eyelids, light sensitivity, and even vision problems if left untreated.
“Ocular rosacea is often linked to blepharitis, a condition where the eyelids become inflamed due to an overgrowth of bacteria or Demodex mites.
“Rosacea keratitis can also develop in the ocular region. This causes painful inflammation at the front of the eye, blurred vision and is usually treated by the patient’s GP.”
She states, “If your patient is experiencing eye-related symptoms, advise them to seek advice from a dermatologist or ophthalmologist. This is because untreated ocular rosacea can lead to complications such as corneal damage.”
It can be useful to build connections in this area so you have a reliable specialist to refer patients on to when necessary.

Should rosacea be treated by an aesthetic practitioner or a dermatologist?
“Many aesthetic practitioners can help manage rosacea symptoms, particularly through non-invasive treatments and skincare advice,” says Dr Carol.
“However, for more severe or persistent cases, such as the presence of papules, or eye or nose involvement, a dermatologist referral may be required. If you’re an aesthetic practitioner trained in skin conditions, you can offer treatments that reduce redness, strengthen the skin barrier, and improve overall skin health.
These approaches to rosacea management are taught on our Cosmetic Dermatology Course. Here you learn all about the ‘skin first’ approach to aesthetics, including skin consultations and popular treatments such as microneedling and polynucleotides.
This certified cosmetic dermatology course can be taken on its own or combined with our industry-leading postgraduate qualification, the Level 7 Diploma in Cosmetic Injectables. Taking this Level 7+ programme prepares you to be a safe, effective and evidence-based aesthetic practitioner with commercially advantageous holistic treatment skills.
From tailoring bespoke skincare routines and treatment plans, to managing common skin conditions including rosacea, acne and hyperpigmentation, and confidently administering botox and fillers using best practice techniques, this aesthetics training sets you up for success. What’s more, our trainees regularly tell us that it’s not only informative – it's fun, too!
The best aesthetic treatments for rosacea
Dr Carol advises, “Several aesthetic treatments can help improve rosacea symptoms by reducing redness, strengthening capillaries, and calming inflammation”
- Laser therapy, such as Intense Pulsed Light (IPL) or vascular lasers: “These can target broken blood vessels and diffuse redness”
- Microneedling: “When performed with caution, this collagen-induction therapy can improve skin texture and barrier function, whilst soothing and nourishing rosacea-prone skin”
- Cosmetic injectables such as Profhilo or polynucleotides: “When considering injectable aesthetic treatments, it’s crucial to choose options that support and strengthen the skin rather than cause further irritation.”
It’s also worth educating your patients on the importance of wearing good quality, broad-spectrum of SPF50 every day, all year round. Certainly, no lower than SPF30 should be considered, and the formulation should be suitable for sensitive skin to avoid irritation. This skincare step is particularly important for rosacea patients as it can help to minimise heat-based flares and redness.
Optimal treatment solutions for patients with both rosacea and acne
“For your patients with both rosacea and acne-like breakouts, treatment must be approached carefully to avoid exacerbating symptoms,” cautions Dr Carol.
“Many of the same treatments used for general rosacea apply, such as laser therapy and LED light therapy. However, additional medical treatments may be needed to control inflammatory papules and pustules.”
Examples include:
- Prescription azelaic acid
- Ivermectin
- Low-dose doxycycline.
Avoid these aesthetic treatments for rosacea patients
When it comes to your standard botox and filler treatments, these are not contraindicated. They’re not going to help manage your patient’s rosacea but if they’re looking for these treatments, you don’t need to worry about
With skin treatments, it’s trickier to navigate, as she explains... “Certain treatments can aggravate rosacea symptoms or cause flare-ups.”
These include:
- Aggressive chemical peels
- Strong retinoids
- Abrasive exfoliating treatments
- High-heat treatments such as radiofrequency or aggressive laser resurfacing, which can worsen redness
- Some active skincare ingredients, including vitamin C and salicylic acid, are best avoided.

What treatment plan would you propose for this patient?
Let’s see how you’d put Dr Carol’s insights into practice!
Meet Susan
Susan is a 56 year old female who’s come to you with a number of aesthetic concerns and you need to put a treatment plan together that addresses all of them.
Background:
- Diagnosed with erythematotelangiectatic rosacea by her GP when she was 32
- Does not take any medication for her rosacea
- Is not aware of any triggers, except heat
- Uses a very basic skincare routine of facewash and moisturiser only
- Her concerns are redness, signs of ageing and “looking tired”.
For the purposes of this exercise, you should assume that Susan is generally in good health and has no budgetary constraints.
What would you recommend for this patient?
We’ll post this – and a follow-up with our advice - to our social media channels. Follow us on Instagram @Harley_Academy or on TikTok @HarleyAcademyOfficial to join in! We'll also post a follow-up to this case with our treatment recommendations and considerations here, so check back for the update to see how you got on...
All information correct at time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners














STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

