How to Avoid Causing Blindness from Fillers

Blindness from fillers is a rare yet critical visual complication that can occur when injecting filler, especially in high-risk areas.
An April 2024 article update published by the Aesthetic Surgery Journal reviews worldwide cases of blindness after filler injections. Researchers in Canada and the USA examined documented visual complications from September 2018 to March 2023.
A total of 365 new cases of partial or complete vision loss were identified.
To understand more about how common blindness from fillers is in aesthetics, we spoke with Dr Emily Mehta. As Harley Academy’s Chief Medical Officer and an aesthetic medicine expert, she offers valuable clinical insights.
Dr Emily also shares what aesthetics practitioners should be aware of when faced with this complication.
Here’s what she had to say…

How common is blindness from dermal fillers?
While blindness from filler is a rare complication, Dr Emily highlights, “This paper only looks at the recorded cases.
“73 cases of blindness from filler were recorded per year, globally, but not all cases are reported.”
This suggests that the actual number of incidents may be much higher.
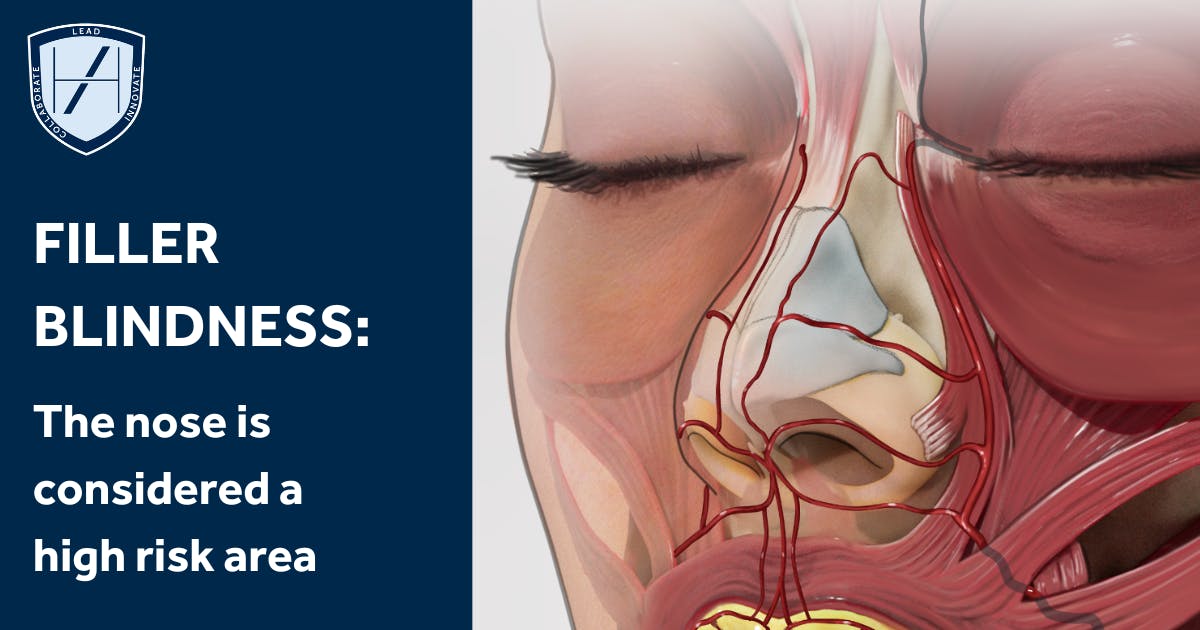
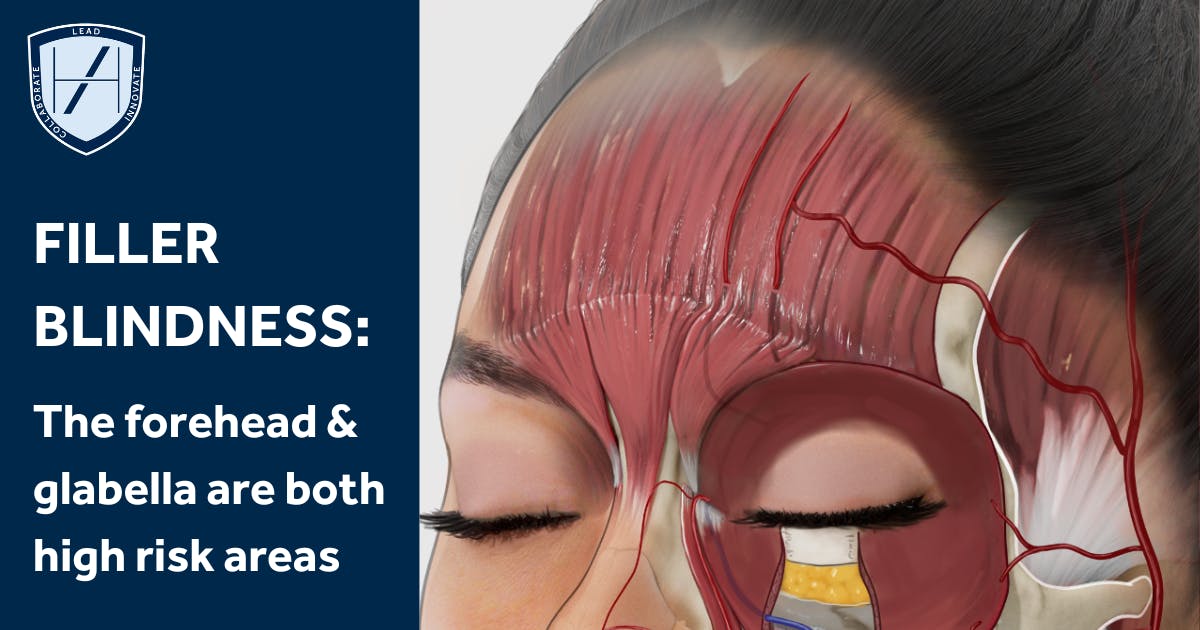
High-risk filler treatment areas associated with potential blindness
Dr Emily explains, “The most common and presumed cause of filler blindness is when a small particle of filler blocks arteries supplying the retina.
“In order, these are the most common treatment areas where this can happen:
- Nose
- Forehead
- Glabella.”
The study also reports that hyaluronic acid was the filler type used in 79.6% of the visual complications reviewed.
What aesthetics practitioners should do if they suspect blindness
We asked Dr Emily, what should an aesthetic practitioner do if a patient experiences blindness? Understanding what signs you should look out for will help you to become a safer and more confident injector.
She gave us a step-by-step guide on what to do in the situation of visual complications post-filler treatment.
“The first thing you need to do is stop treating,” she urges.
“Second is to ask the patient a few quick questions to assess what’s going on and examine the situation.
Here are some symptoms Dr Emily confirms you need to look out for:
- Eye pain
- Nearby skin ischemia
- Description of reduced vision in one eye
- Ophthalmoplegia - the eyeball veering towards one side or getting double vision
- Ptosis - eyelid droop, which is a symptom that’s present half the time and recorded in this paper
- 1 in 5 patients can experience mild symptoms of stroke, so check for any neurological symptoms such as weakness of hands, legs or change in speech.
“If any of these are happening, stop injecting and get the patient to A&E as soon as possible,” she insists. “Preferably, you want to take the patient somewhere with a specialist eye department or an emergency eye hospital.”
How to manage patients with potential filler blindness symptoms
As mentioned above, your first priority on presentation of relevant symptoms is to get your patient to A&E immediately.
There are several steps you can take to help manage the situation in the period between identifying concerns and arriving at A&E.
These should not delay getting the patient to A&E immediately.
Medical steps
Dr Emily suggests, “While waiting for the patient to be taken to A&E you can apply ocular pressure. This may help the profusion of the retina. You can do this by gently pressing on the closed affected eyelid.
“If on hand, you can also give the patient 300mg of aspirin as you would in any ischemic episode. However, it’s important to note that none of this should delay getting the patient to A&E.”
Dr Emily stresses, “We do not advise giving any hyaluronidase yourself. From the recorded cases in the study, unfortunately, there is no evidence that applying hyaluronidase improves vision outcomes.”
She adds, “It’s worth noting that, because blindness from filler is rare, if the patient does develop symptoms after filler treatment, it’s still as likely - or more likely - that it may not be from the filler treatment. It’s advised you do not administer any treatment yourself.”
Psychological steps
This will be an incredibly unnerving experience for your patient. As such, do your best to keep them calm and informed.
Whilst it’s always good practice to ensure your patient feels reassured when dealing with complications, ensure you’re realistic.
Never make promises regarding outcomes or downplay the potential severity of an issue.
Helping them to understand what steps you’re taking, why and that you’re proactively managing the process can be comforting.
This transparent approach will not suit all patients so, as always, tailor your communication to the individual. Just remember to be empathetic even though it will be a stressful situation for you too.
How to avoid causing blindness from filler when injecting
When we asked Dr Emily how aesthetic practitioners can avoid causing filler blindness when injecting, she offered three key points:
1. Avoid high-risk treatment areas
“Don’t inject high-risk treatment areas, that’s the best thing you can do to avoid it!”
2. Acquire the proper knowledge
“If you’re injecting filler in those high-risk areas, such as the nose and forehead, make sure you're properly trained. Know your anatomy and inject very small quantities.”
3. Refuse treatment to patients with unilateral blindness
“Another thing you can consider is not injecting patients who are already blind in one eye. This is the stance that Harley Academy takes.
“The reason for this is that the impact on quality of life for complete bilateral blindness is much worse than unilateral. If you have blindness in one eye, you can still live a relatively normal life.
“If you’re blind in both eyes, there’s a severe impact on your quality of life. So a way of mitigating that scenario from happening is not treating patients who are already blind in one eye.”
Extensive medical aesthetics training in high-risk areas
“The three treatments identified in the article as the highest risks should only be administered by experienced injectors. However, the practitioner’s skills and aesthetics training are as important, if not more, than experience,” Dr Emily underscores.
She continues, “Some aesthetic practitioners have been injecting for a long time so are experienced, but they’ve been injecting wrongly.
“We advise, if treating these areas, you have experience, confidence and in-depth aesthetics training in these regions. This is especially the case for the glabellar – we don’t recommend doing filler treatment at all here. Meanwhile, for injecting filler in the forehead, we recommend using a cannula!”
Learning to use a cannula is a great way to reduce bruising and vascular complications. Reserved for aesthetic medicine practitioners who are confident in their needle techniques, we teach cannula use in many of our courses.
Our Injectables Masterclasses, for example, target popular treatment areas and encourage cannula use. These are the regions aesthetic practitioners are frequently looking to increase their knowledge and techniques in.
As you practice your injecting and continue topping up your training, you’ll gain confidence and mastery. This, in turn, will allow you to create natural-looking results that attract and maintain long-term patients.
Common mistakes when injecting filler in high-risk areas
It’s important to mention here that forehead, nose and glabella filler treatments are not currently taught at Harley Academy.
Dr Emily reports that common mistakes when injecting filler in these areas are usually centred around:
1. Injecting at the wrong depth
2. Injecting the wrong amount of filler product.
Non-surgical rhinoplasty and forehead fillers are incredibly specialist areas of practise. These should certainly never be attempted by anyone without the proper practical training where injection depth and dosing will be taught.
How concerned should injectors be about causing filler blindness?
We wanted to know if aesthetics practitioners should be worried about causing filler blindness when injecting. This concern is one we frequently hear from new injectors and medics considering entering the field who are scared of causing such complications.
But what are the realities of this fear? How worried should you be about potentially causing filler blindness?
Dr Emily told us, “If you’re not injecting those high-risk areas, then your worry levels can be low. However, as an aesthetics practitioner, you must accept that this is a possible outcome of filler injections anywhere in the face.
“I often hear practitioners say when consenting their patients that there is a theoretical risk of blindness - this is not true! There is a literal risk of blindness, it’s just a very, very low risk.
“Furthermore, it’s not something you need to be concerned about with every injection. It’s important to ensure you’re treating areas that you’re trained to do competently, in a way that minimises vascular ischemia or embolism. Also, knowing your anatomy is crucial!
“You do, however, need to be prepared to take responsibility for that risk. Be ready to discuss it with your patient so they can give informed consent.”
We hope this real-world advice from a true aesthetics expert helps to put your mind at rest!
There are risks of complications associated with any medical procedure. It’s how you prepare to prevent and manage them via your on-going education and regularly updated protocols that’s important.
All information correct at the time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners












STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services


