An Injectors' Guide to Filler-Related Nodules

Dermal filler-related nodules can be a scary topic for aesthetics practitioners, not to mention a highly involved one
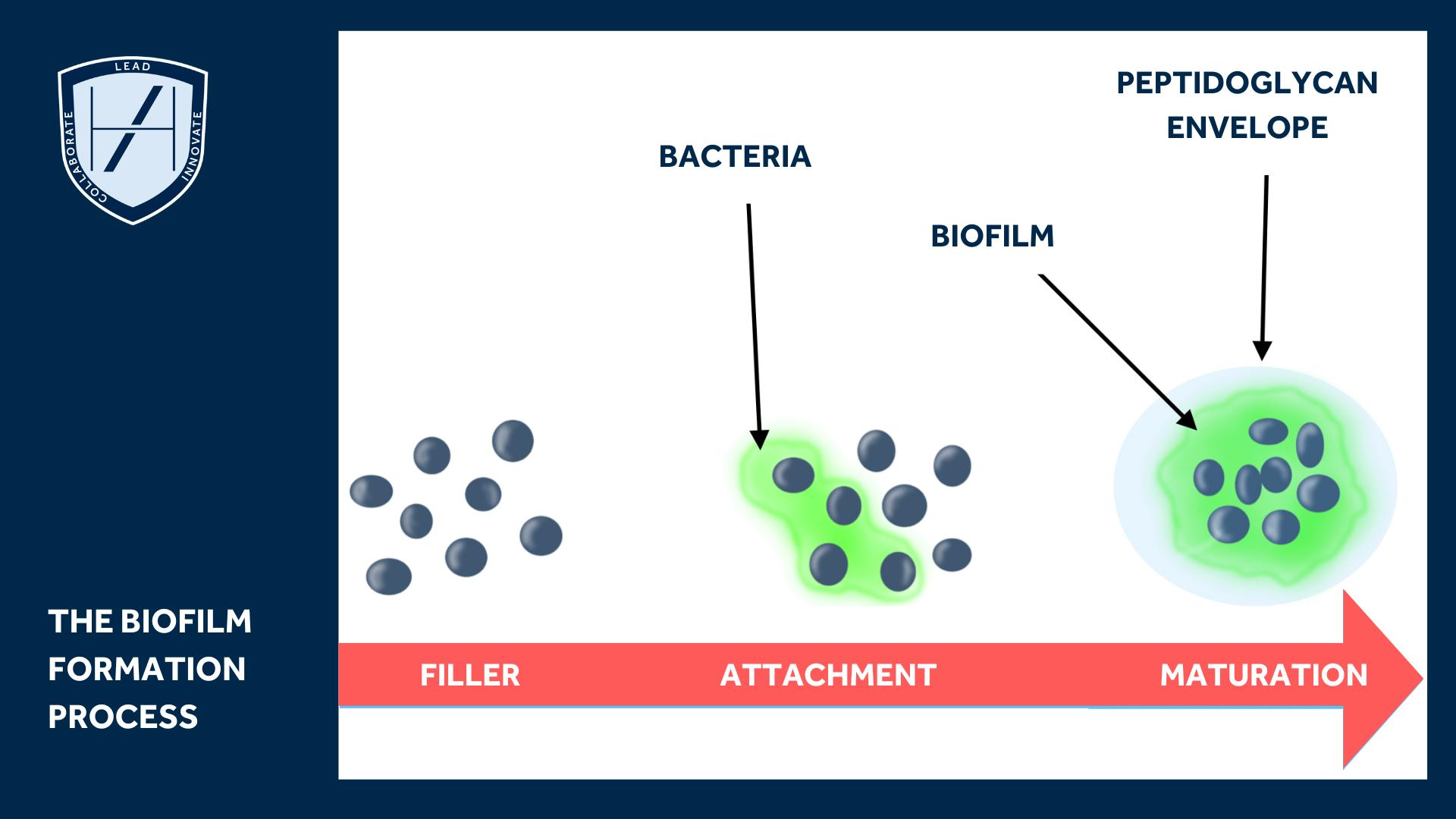
Delayed onset nodules (DONS) are often seen as difficult and confusing complications. DONs is not a diagnosis, it simply describes nodules that occur after dermal filler treatment. Nodules can be non-inflammatory or inflammatory in origin, with biofilm thought to be involved in both types.
Our Chief Medical Officer, Dr Emily Mehta, explains that a nodule is a “lump or induration present at least two weeks after filler injection”. She notes that, while this may be a description, it is not a diagnosis.
This article addresses non-inflammatory nodules, delayed hypersensitivity nodules and inflammatory nodules from a medical aesthetics perspective. We focus on their early signs, prevention and treatment in relation to new research into non-ischaemic complications of dermal fillers.

Recent literature review of filler-related nodules
A narrative literature review in the Plastic and Aesthetic Research journal suggests “Inflammatory nodules are secondary to infection or foreign body reactions.” While “non-inflammatory nodules are due to superficial injections or improper filler placement.”
Bear in mind that the advice from any paper needs to be considered in context. This means in the context of all the available evidence, and that of the individual. If in doubt, it’s always appropriate to seek further advice on managing clinical complications you’re unfamiliar with.
Understanding filler-related nodules, their prevention and potential management, is a complicated subject. This is not something many new aesthetics practitioners get to grips with early on in their careers. However, it’s a significant matter that it’s never too early to start being aware of.
Non Inflammatory Nodules
The review suggests that non-inflammatory nodules are secondary to “overcorrection or erroneous placement of filler.” They are not associated with signs of inflammation, like erythema and swelling.
If hyaluronic acid fillers are used, non-inflammatory nodules can be dissolved using hyaluronidase.

Inflammatory nodules
The review authors propose various reasons for these reactions including infections, immunogenic triggers and HA-breakdown byproducts. However, the exact aetiology is multifactorial.
“The pathophysiology of these nodules involves T-lymphocytes and macrophages”, the study notes. These reactions can occur anywhere from 24 hours to several months after injection. These filler-related nodules can also progress to a specific granulomatous reaction.
These are filler-related nodules secondary to infection or foreign body reactions.
Infection
Early signs of infection can appear as fluctuant and tender lumps only a few days after injection.
The aforementioned review notes that the “risk of infection does not appear to be dependent on filler type but more on breaks in sterile technique.
“These infections are secondary to Staphylococcus aureus, but can also be caused by other viral and fungal species such as Candida.”
Management options
This can be managed with an incision, drainage and general cephalosporins.
If an abscess is present, it’s recommended that an incision and drainage be carried out. Cultures and antibiotics are also advised.
Massage or treatments with hyaluronidase should be avoided until infection is cleared. Massage may mechanically spread infection. Hyaluronidase use breaks down tissue and this may also spread the infection further.
Importantly, “Patients who have developed midfacial and periorbital infection should be monitored for intracerebral complications”, the study authors note.
If a late infection occurs after two weeks, it may be secondary to atypical mycobacteria. These mycobacteria are often drug-resistant and very difficult to treat. Experts recommend obtaining bacterial cultures for these late-onset infections and performing sensitivity reports to help tailor the antibiotic regimen.

Delayed hypersensitivity nodules
What are delayed hypersensitivity nodules?
Often described as “angry red bumps”, delayed hypersensitivity nodules occur in the area of the filler injection. They are characterised by induration, erythema and oedema.
Aetiology of these filler-related nodules is unknown
The researchers advise, “An increase in proinflammatory levels of C-reactive protein, fibrinogen, and angiotensin convertase (which appears to also play a role in delayed nodules after COVID-19 reactions) have been seen in patients with delayed hypersensitivity reactions.”
However, one study the paper notes showed 12 patients who’d experienced a delayed hypersensitivity reaction and underwent intradermal testing. They didn’t experience any reaction. This suggests type I and type IV hypersensitivity don’t play a role in these late inflammatory reactions. However, an element of the inflammatory process could be causing these nodules.
In one of the author’s experiences, an example suggests anything that “flares up the immune system, including dental work, cutaneous surgery/lasers, sinus infection, UTI, irritable bowel syndrome, or autoimmune conditions, can lead to the presentation of these nodules.” These normally resolve in 1-2 days with diphenhydramine or doxycycline at an inflammatory dose.
Another possible aetiology for these nodules includes filler byproducts. Hyaluronic acid is not typically immunogenic, but other components that stabilise these molecules may predispose the filler to become immunogenic. It’s also been theorised that glycosaminoglycans can act as superantigens and active immune reactive cells.
“After changes in the manufacturing process reduced the protein load in HA by six-fold, the incidence of inflammatory reactions decreased from 0.15 to 0.06 per cent.”
May lead to granulomas
Delayed hypersensitivity nodules can lead to granulomas. A granuloma is considered a form of chronic inflammation which can only be diagnosed histologically. They occur in response to foreign material that has been unable to be phagocytosed by macrophages.
Various factors can increase the chances of granulomas. One study found an irregularity in the particle surface may cause a longer-lasting inflammatory reaction and severe systemic infection.
The review notes that a relationship between biofilms and granulomas has been considered. However, the topic is still up for debate.
Other things that lead to the development of granulomas include “superficial placement, hydrophobic polymer gels, smaller particle size, volume of the filler, intramuscular injection and previous infections.”
Treatment of granulomas
The treatment aim with granulomas is to stop the cell invasion and interstitial substance secretion. Infection must be ruled out with bacteriological sampling before starting steroids and immunosuppressant treatment. Hyaluronidase, steroids, 5-FU injections and triamcinolone injections should be considered. This would usually be in a specialist setting.
The review authors advise, “If a patient presents with a late inflammatory nodule, and there is fluctuation, incision and drainage should be performed to assess for infectious causes”.
If there is no clinical improvement after 1 week, biopsy specimens should be assessed for histopathology and microbiological cultures. Antibiotics should also be continued for several weeks.
Understanding Filler-Related Nodules
As you grow as a medical aesthetics practitioner, you’ll need to understand more about the various filler-related nodule types. Developing a confident knowledge of how to prevent, identify and manage complications, such as those outlined above, will elevate the safety of your practice.
We cover such complications in our Ofqual-regulated and JCCP-approved Level 7 Diploma in Botox & Dermal Fillers course.
Additionally, we have a standalone eLearning course available to doctors, dentists and nurses outside of our Level 7. This helps you to specifically understand Preventing and Managing Dermal Filler Complications using case studies.
To find out more about the learning opportunities that fit best with what you’re looking to achieve in your aesthetics career, contact our Course Advisors today.
All information correct at the time of publication
Download our full prospectus
Browse all our injectables, dermal fillers and cosmetic dermatology courses in one document
By submitting this form, you agree to receive marketing about our products, events, promotions and exclusive content. Consent is not a condition of purchase, and no purchase is necessary. Message frequency varies. View our Privacy Policy and Terms & Conditions
Attend our FREE open evening
If you're not sure which course is right for you, let us help
Join us online or in-person at our free open evening to learn more
Our Partners












STAY INFORMED
Sign up to receive industry news, careers advice, special offers and information on Harley Academy courses and services

